ODI’s theory of change
The ODI is consciously evolving in order to meet the needs of an increasingly complex and data-enabled world.
We have defined six guiding principles for the next five years that are rooted in our core identity (our vision and mission), our position in the world and our unique body of knowledge and expertise.
Health data is a term used to describe all the information generated
through the process of delivering healthcare to populations, including
disease registries, public health surveys, clinical trial data,
insurance claims and electronic health records.
Primary use of health data is when health data is used to deliver healthcare and to make decisions about the care of the individual from whom it was collected.
Secondary use of health data is the use of aggregated health data from population-level sources – such as electronic health records, health insurance claims data and health registry data – to improve personal care planning, medicines development, safety monitoring, research, and policymaking.
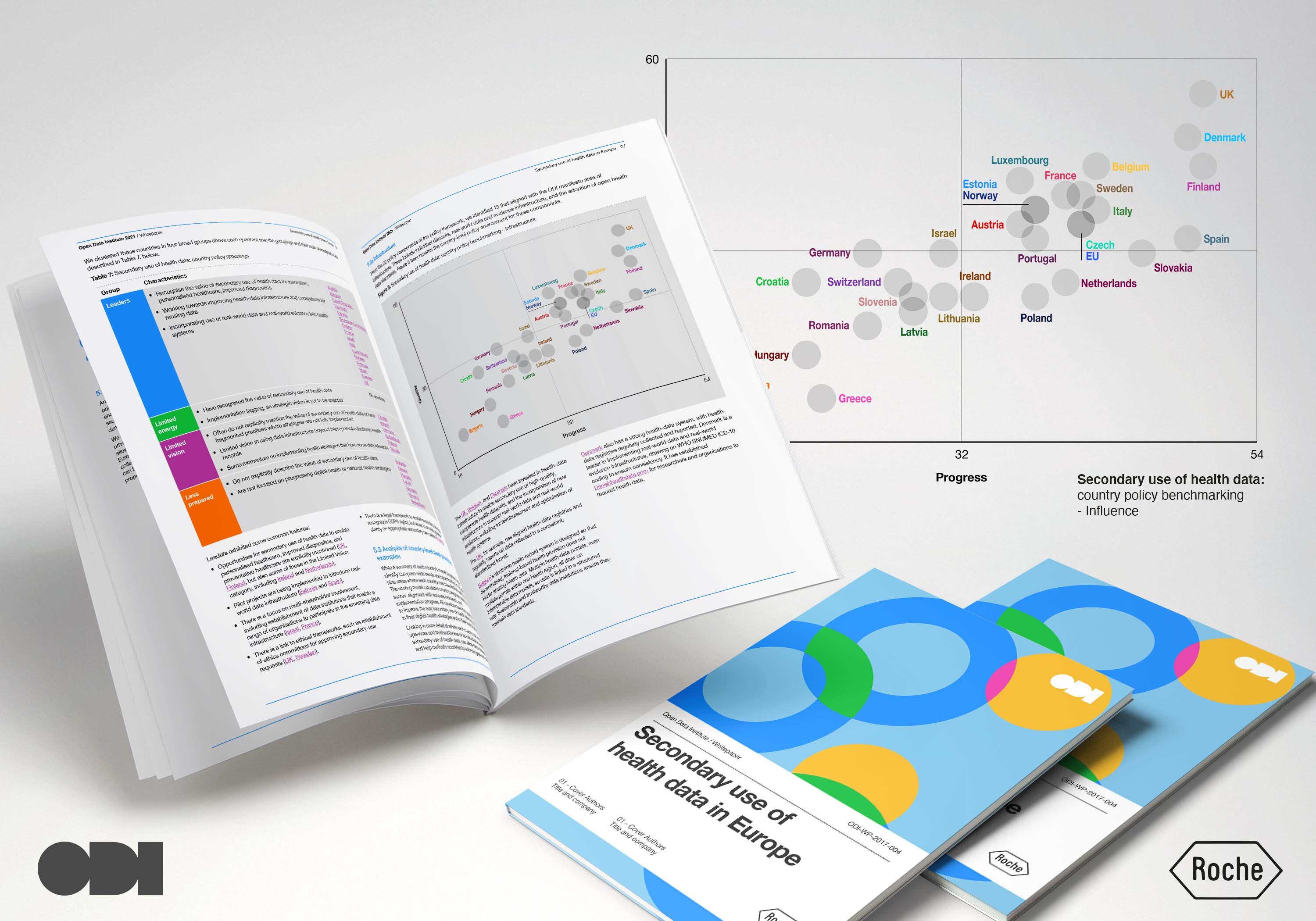
During our 2021 research and policy analysis on secondary use of health data policy approaches across governments,
a team, lead by Dr Milly Zimeta and including Mark Boyd as lead author alongside Jeni Tennison and Mahad Alassow,
developed a policy framework model with 22 key policy components needed to needed to achieve an open and
trustworthy data ecosystem, aligned with the ODI's six manifesto points. In 2023, the ODI updated its manifesto by
building the points into a set of six principles as part of its new Five Year Strategy. As a result, the secondary use of
the health data policy framework was similarly updated to reflect these new principles (see Table 2 in our Western
Balkan nations report).
For each policy component, we proposed a ‘success indicator’ – a one-sentence statement explaining how it would operate if it was a fully functional policy area. Finally, we evaluated these success indicators in two ways:
Download detailed Annexe: Methodology
We have defined six guiding principles for the next five years that are rooted in our core identity (our vision and mission), our position in the world and our unique body of knowledge and expertise.
- Principle 1 We believe that a strong data infrastructure is the foundation for building an open, trustworthy data ecosystem on a global scale and that this can help address our most pressing challenges.
- Principle 2 Strong data infrastructure includes data across the spectrum, from open to shared to closed. 2 But the best possible foundation is open data, supported and sustained as data infrastructure. Only with this foundation will people, businesses and governments be able to realise the potential of data infrastructure across society and the economy
- Principle 3 For data to work for everyone, it needs to work across borders – geographic, organisational, economic, cultural and political. For this to happen ethically and sustainably, there needs to be trust – trust in data and trust in those who share it.
- Principle 4 There is greater need than ever for trusted, independent organisations to help people across all sectors, economies and societies to benefit from better data infrastructure.
- Principle 5 For data to work for everyone, those collecting and using it need to be highly alert to inequalities, biases and power asymmetries. All organisations working in data must take proactive steps to ensure that they contribute fully and consciously to creating a diverse, equitable and inclusive data ecosystem.
- Principle 6 The world needs a new cohort of data leaders – individuals who have data knowledge and skills and are equipped to understand the value, limitations and opportunities offered by data, data practices and data sharing.
Policy for secondary use of health data
Primary use of health data is when health data is used to deliver healthcare and to make decisions about the care of the individual from whom it was collected.
Secondary use of health data is the use of aggregated health data from population-level sources – such as electronic health records, health insurance claims data and health registry data – to improve personal care planning, medicines development, safety monitoring, research, and policymaking.
For each policy component, we proposed a ‘success indicator’ – a one-sentence statement explaining how it would operate if it was a fully functional policy area. Finally, we evaluated these success indicators in two ways:
-
What is the quality of policy activity for this success indicator?
The scoring range for evaluation of activities is:
○ Having only limited aspects of the success indicator (low / 0);
○ Aligned intent but missing key aspects (medium / 2);
○ Fully comprehensive (high / 4). -
What progress is being made on implementation of policy for this
success indicator?
The scoring range for implementation of activities is:
○ Not started (0);
○ Defined (1);
○ Planned (2);
○ Pilot initiatives (3);
○ Scaled-up implementations (4).
All the data in our report was correct as of October 2023.
Download detailed Annexe: Methodology